High Tibial Osteotomy for Knee Osteoarthritis
Knee osteoarthritis is a leading cause of disability, especially in active individuals under 60.
When arthritis predominantly affects the inner (medial) compartment of the knee, High Tibial Osteotomy (HTO) can be a valuable joint-preserving surgical option. Dr Daniel Meyerkort, orthopaedic surgeon at Perth Orthopaedic & Sports Medicine, specialises in both surgical and non-surgical treatments for knee osteoarthritis, helping patients delay or avoid total knee replacement and return to active lifestyles.
This article will provide a detailed look at knee osteoarthritis management, focusing on high tibial osteotomy, the benefits and risks, and how Dr Meyerkort’s tailored approach supports patients in Perth and across Western Australia.
Understanding Knee Osteoarthritis
Osteoarthritis (OA) is a degenerative joint condition where cartilage breaks down, leading to joint pain, stiffness, swelling, and reduced mobility. In the knee, OA may be unicompartmental, affecting only one section—most commonly the medial compartment, which is the inner part of the knee.
Risk factors include:
Age
Obesity
Previous injuries such as meniscal tears or ACL ruptures
Malalignment of the lower limb (varus or bow-legged alignment)
When the alignment is off, more stress is placed on the medial side of the knee, accelerating cartilage wear. That’s where High Tibial Osteotomy (HTO) comes into play.
Non-Surgical Management of Knee Osteoarthritis
Before considering surgery, Dr Meyerkort explores a range of non-surgical options to manage symptoms and improve function. These include:
1. Activity Modification and Weight Loss
Reducing high-impact activities and achieving a healthy weight can decrease the mechanical load on the knee. For every 1kg of weight lost, the knee experiences a 4kg reduction in load during walking.
2. Physiotherapy
Targeted physiotherapy helps strengthen the quadriceps, hamstrings, glutes, and calf muscles. Improved muscle support reduces joint stress and improves knee stability.
3. Bracing
Unloader braces are designed to shift the load from the medial compartment to the lateral compartment, offering pain relief during activity.
4. Medications
NSAIDs such as ibuprofen or meloxicam for inflammation and pain
Paracetamol for general pain management
5. Injections
Corticosteroid injections for short-term inflammation control
Hyaluronic acid injections (viscosupplementation) to lubricate the joint
Platelet-Rich Plasma (PRP) injections—offered by Dr Meyerkort at Perth Orthopaedic & Sports Medicine—for biological cartilage support and inflammation reduction
If these methods are insufficient, and the patient is still active with isolated medial knee OA, HTO becomes a surgical consideration.
What is High Tibial Osteotomy?
High Tibial Osteotomy (HTO) is a joint-preserving procedure where the tibia (shinbone) is cut and realigned to offload the diseased compartment of the knee. This shifts the body weight away from the damaged medial side towards the healthier lateral compartment.
HTO is most suitable for:
Patients aged 40–60
Isolated medial compartment OA
Good range of motion and stable ligaments
Physically active individuals wanting to delay total knee replacement
Surgical Procedure: High Tibial Osteotomy by Dr Daniel Meyerkort
Dr Meyerkort performs HTO using advanced techniques at Perth Orthopaedic & Sports Medicine. The surgery involves:
Planning: Using long leg alignment X-rays and CT scans to precisely calculate correction angles.
Surgical Technique:
Opening wedge osteotomy (most common): A wedge is created on the inner tibia, opened to a specific angle, and stabilised with a titanium plate.
Closing wedge osteotomy: Bone is removed from the outer tibia, and the gap is closed.
Internal Fixation: The tibia is stabilised using plates and screws, allowing for accurate healing.
Rehabilitation: Weight-bearing is usually limited initially, followed by a structured physiotherapy program.
Dr Meyerkort uses cutting-edge imaging, planning software, and modern implants for optimal outcomes.
Benefits of High Tibial Osteotomy
1. Joint Preservation
HTO maintains the native knee joint and defers the need for total knee replacement, particularly beneficial for younger, active patients.
2. Pain Reduction
By realigning the leg and offloading the affected compartment, patients often experience significant pain relief.
3. Return to Activity
HTO allows patients to resume sports, work, or physical hobbies that may be restricted after a total knee replacement.
4. Delays Knee Replacement
HTO can delay or avoid knee replacement surgery by 5–10 years, or more in some cases.
5. Natural Joint Function
Patients retain better proprioception and joint mechanics compared to joint replacement.
Risks and Complications of HTO
As with any surgery, there are risks, although complications are uncommon when performed by an experienced surgeon like Dr Meyerkort. These may include:
Infection: Treated with antibiotics or surgical washout
Non-union or delayed bone healing
Over- or under-correction of alignment
Deep vein thrombosis (DVT)
Plate irritation requiring later removal
Progression of OA: May still require knee replacement in the future
Careful pre-operative planning, surgical precision, and postoperative rehabilitation help mitigate these risks.
Recovery After High Tibial Osteotomy
Patients typically stay one to two nights in hospital. Initial recovery involves:
Crutches for 6–8 weeks
Progressive weight-bearing
Physiotherapy to restore motion and strength
Return to low-impact activities by 3–6 months
Full return to sport usually by 9–12 months
Dr Meyerkort provides a tailored rehab plan and ongoing review at Perth Orthopaedic & Sports Medicine.
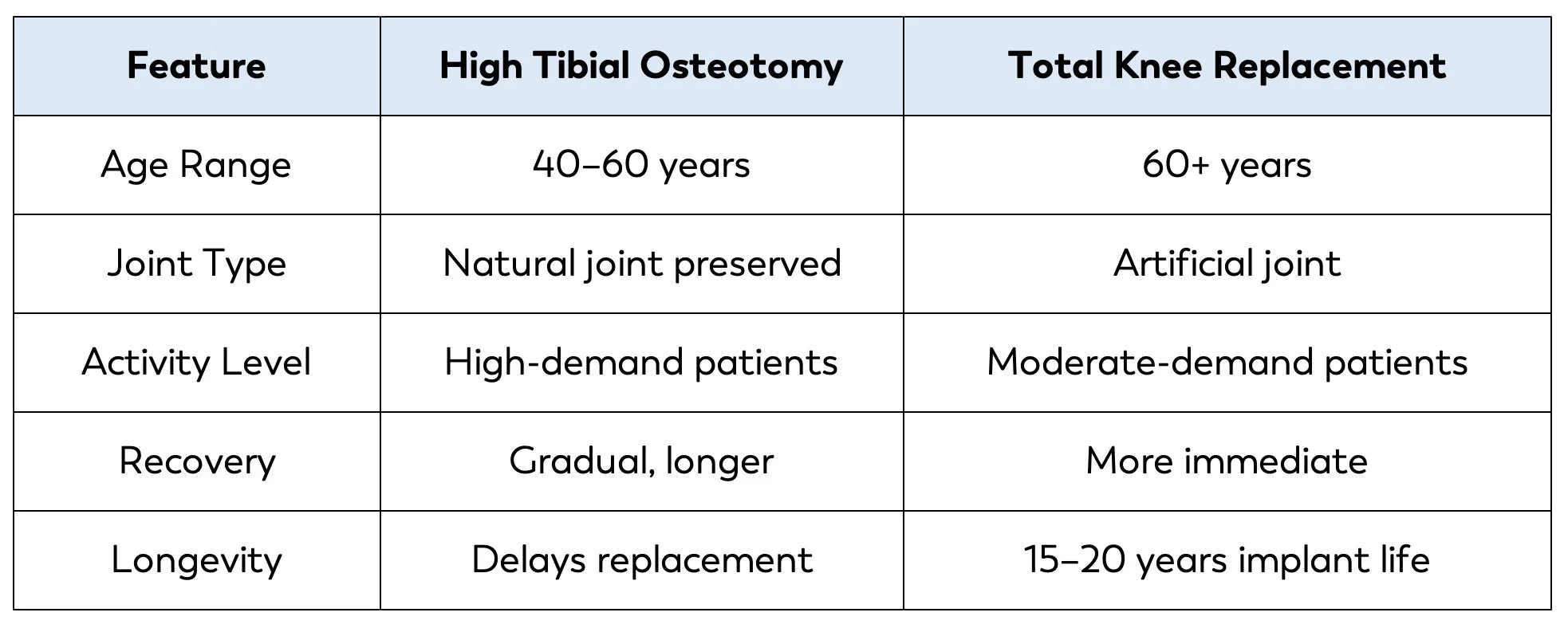
High Tibial Osteotomy vs. Total Knee Replacement
HTO is ideal for those wanting to stay active, especially in jobs or sports requiring deep knee flexion.
Why Choose Dr Daniel Meyerkort for HTO in Perth?
Dr Daniel Meyerkort is a fellowship-trained orthopaedic surgeon specialising in knee osteotomy and cartilage preservation surgery. At Perth Orthopaedic & Sports Medicine, patients benefit from:
Comprehensive assessment and advanced imaging
Individualised non-surgical and surgical management
Access to biologic injections (PRP, HA)
Precision surgical techniques with modern implants
Collaborative care with physiotherapists and sports medicine physicians
Dr Meyerkort is committed to restoring knee function and delaying joint replacement, using the latest evidence-based techniques.
Personalised Orthopaedic Care in Perth
Whether you are based in Perth, rural WA or regional towns, you can access expert care for knee osteoarthritis. Telehealth consultations are available to discuss imaging, assess suitability for HTO, and create a treatment plan tailored to your lifestyle.